
What is contact eczema?

An allergic reaction
Contact eczema presents all the usual eczema symptoms, in particular those all-too-familiar itchy red patches... Its cause, however, is very specific: an allergic reaction to a product or object coming into contact with the skin.
The most common example is an allergic reaction to costume jewelry, but others are more difficult to diagnose.
Recognizing contact eczema
Contact eczema is a form of skin inflammation which occurs on areas of the body that have been directly exposed to the allergen and/or near the area of initial contact. Once contact eczema has been diagnosed, the next step is to identify the triggering agent. This could be nail polish, clothing, a fragrance, paint or an industrial oil, to name a few examples.
Symptoms
Below are the symptoms associated with contact eczema:
- Red patches
- Itching
- Oozing
The severity of symptoms varies greatly from one person to the next, but inflammation always develops in the same order: erythema (redness) with possible edema (swelling) > vesicles (little blisters) > oozing (from blisters opening) > scabs
Persistent eczema causes the appearance of affected areas of the skin to change: it becomes thick, dry, hyperkeratotic, scaly, and oozing (although rare and barely visible). Of course, we see variations in terms of the severity of edema, vesicles and peeling and in terms of localization.
Symptoms may appear several days after exposure to the allergen. This means you may need to think back to uncover what may be irritating your skin.
It's possible to develop a "sudden" allergy
You can suddenly become allergic to something that, up until now, you tolerated perfectly well. Contact eczema can, therefore, appear with the hundredth or even thousandth exposure to the allergen, without any prior history of an allergy.
Initially, eczema appears on the area in direct contact with the triggering agent, but, if exposure continues, it may affect other areas or even become widespread.
The various types of contact
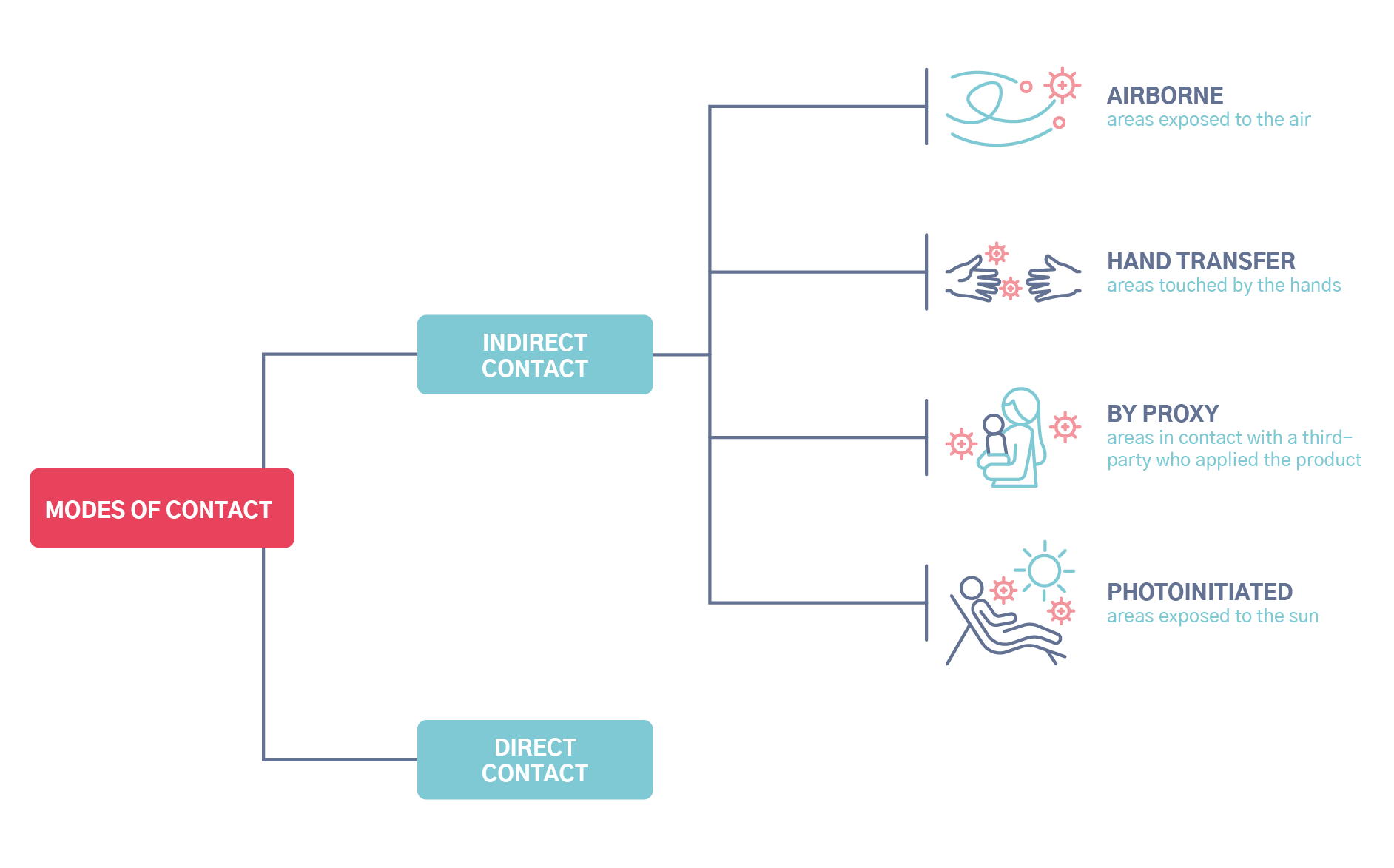
Eczema versus a simple irritation
Not all skin reactions to products or objects are contact allergies. Redness can be a sign of a simple irritation, without being full-blown eczema, especially with personal care products and the like.
What should you do if you have contact eczema?
You will likely need to undergo treatment which involves applying a topical corticosteroid over the course of a few days until your symptoms clear up. At the same time, you will need to identify the cause, or contact allergen, in order to eliminate or avoid it and thus prevent recurrence.
Identifying the cause of your contact eczema
To find out what could have caused this allergic reaction, the first step is to thoroughly investigate what may have come into contact with this exact area of your body prior to the onset of eczema. The answer lies in how you respond to a number of questions:
“What did you apply to that area before symptoms began?”
“Have you done any home improvements over the last two or three days?”
“Have you been in the sun in recent days?”
Sometimes you remember: it was the earring, jeans button, a cosmetic, paint, clothing, footwear... But sometimes you don’t.
Unless the cause is obvious, it is important to consult a specialist in dermato-allergology. They will help you investigate and conduct skin tests known as “patch tests”.
Where on the body does the eczema appear? Allergy investigation
The area where redness appears provides valuable insight into the possible cause. For example, eczema on the feet is much more likely to be caused by footwear than by toothpaste. That said, no stone should be left unturned. In the case of an allergy to nail polish, for example, you can develop a reaction on your neck if you touch it often with your hands.
List of the most common contact allergens
The following are objects and products often associated with allergies, along with the triggering allergen.
Scalp: Hair dye (very common), perms, shampoos, other hair care products
Face: Cosmetics (preservatives, fragrances, etc.), personal care products, topical medicines, sunscreens (photoallergies aggravated by sun exposure), airborne allergens (in the air: aerosol fragrances, resins, etc.)
Eyelids: Eye drops, cosmetics, nail polish, airborne allergens
Lips: Cosmetics, medicines, toothpaste, musical instruments
Ears: Jewelry, topical medicines
Neck: Cosmetics, hair care products, jewelry, nail polish
Underarms: Deodorants, clothing
Chest: Undergarments
Hands: This is the trickiest area; we touch so many things at home, at work and in our day-to-day activities!
Legs: Topical medicines, bandages, clothing
Feet: Leather-tanning agents, adhesives, dyes in footwear
“Certain professions are thus more problematic for some people: hairdressers, housekeepers or even lathe and milling machine operators are exposed to more recognized allergens than, for example, a radio host. You may learn about this as part of your career counseling. If you already work in one of these professions, you can find information about how to manage work-related contact eczema with the occupational health services.”
Identifying the cause through allergy testing
You may have heard of patch tests under a different name, such as epidermal tests. This approach to allergy testing is painless as it requires no pricking. It involves placing a series of allergens or products on the back to observe which ones trigger a small eczema patch. You should expect to do about 20 tests to cover the most common allergens (standard battery). The doctor will be able to complete targeted tests adapted to your daily activities or profession.
Have you identified the allergen? Then your problem is solved, as long as you can easily avoid contact with the allergen. If avoidance is impossible (e.g.: a hairdresser who is allergic to hair dye), protection and management solutions are usually available: consult with your dermatologist or occupational physician if the triggering allergen is used as part of your work. When it comes to allergies to a cosmetic ingredient, eliminating the allergen can sometimes be tricky; it involves complex chemical names, and reading labels is difficult.
When you highly suspect an allergy to a specific product which tests negative, the dermato-allergist may have you complete a Repeated Open Application Test, or ROAT. This consists of applying the product for several days on a small area of the forearm. If no reaction occurs, you can do a use test, particularly for cosmetics.
Can you have contact eczema on top of atopic eczema?
Yes. Someone already affected by atopic eczema may also develop contact eczema. This makes diagnosis even more complicated, as atopic eczema is often confused with contact eczema. The rule of thumb for people with atopic skin:
Be careful about what you apply to your skin! When it doubt, test it out.
Allergens pass through atopic skin more easily. It is best to opt for personal care products or skin care with the fewest ingredients possible. Be mindful that “organic” or “natural” provide no guarantees against allergies: essential oils and fragrances, for example, contain common components that can trigger allergies.




