
Eczema on the eyes

Around the eye or on the eyelids are very common places for eczema to appear.
Eye eczema may be caused by an allergy, or it could be one of several possible manifestations (along with asthma) of atopy, a genetic hypersensitivity to the environment.
What does eczema on the eyelids look like?
Do you have an irresistible urge to scratch your eyes? It could be eczema.
If your eyelids are red, swollen, at times oozing, and extremely itchy, then you have acute eczema. Sometimes the skin is simply dry and slightly red, but still itchy.
Eczema or allergic conjunctivitis?
It can sometimes be difficult to tell the difference between eczema and allergic conjunctivitis: in the latter case, eyelids may be a bit swollen and itchy, but the eye is red.
Eczema or psoriasis? Eczema patches are often thinner and their edges less defined compared to psoriasis. Click here for a summary of the major differences between eczema and psoriasis.
Allergic eczema on the eyelids
The skin on the eyelids is very thin and is commonly affected by so-called allergic “contact” reactions to products or objects.
Common causes of allergies
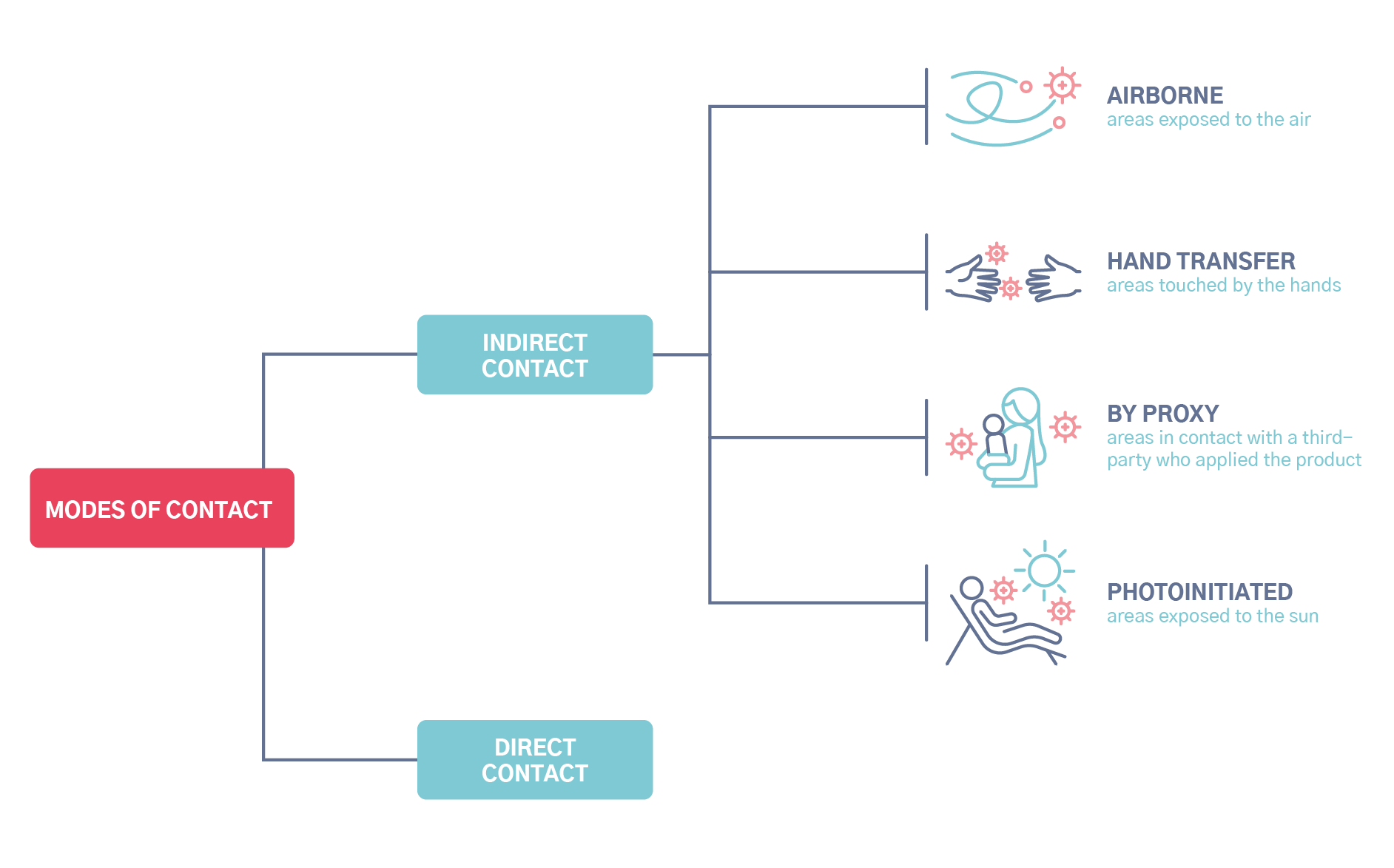
Direct contact

A product comes into direct contact with the eyes or eyelids and triggers an allergic reaction:
- All creams, especially those for the eye contour area
- Shampoo
- Hair dye
- Topical medicines: Eye drops, eye ointments
- Personal care products, make-up removers
Contact via the hands

Eczema can be triggered by indirect contact through the hands.
We often touch or rub our eyes with our hands. The reaction may be caused by a product which has been applied to the hands or which the hands have touched.
- Nail varnish
- Personal care products
- Skin care creams
- Medicated creams or ointments applied to an area of the body
- Metal objects
- etc.
Contact via a third-party

Eczema can be triggered by indirect contact by proxy.
Sometimes, a person can act as an intermediary, transferring the allergen onto the eyelids. For example, a mother who has dyed her hair who then touches the face of her child may cause the child to develop allergic eczema on the eyelids.
- Nail polish (on another person)
- Personal care products
- Creams
Allergen is spread through the air

Eczema can be triggered by airborne allergens.
The eyelids are especially vulnerable to this type of contact.
- Diffused fragrances: home fragrances or aerosol fragrances used in lavatories or bathrooms
- Wood dust
- Certain plants
How do you determine the cause of the allergy?
You will need to remove the allergen from your daily routine, as well as any products or objects likely to contain the allergen. Take varnish for example; it is not the varnish itself that is causing the allergy, but rather an allergen found in the varnish!
Identifying the culprit can be a complex task: the allergic reaction may appear long after the initial exposure or following indirect contact (hands, air, etc.). Consult a doctor specializing in dermato-allergology. They will be able to guide your search and confirm any suspicions.
The doctor will conduct a thorough investigation by asking you questions on your habits at home and at work. They will also carry out allergy patch tests to identify the allergen or allergens responsible.
An allergic reaction is caused by an allergen, or molecule, and not by the object or product itself. With costume jewelry, for example, the allergy is to nickel.
Atopic eczema around the eyes
The primary difference separating atopic eczema from contact eczema is the cause. Atopic eczema is not due to an allergy but rather to atopy, a genetic hypersensitivity to the environment. The eyelids are a common area for atopic dermatitis to appear. It can sometimes be tough to distinguish between all these conditions, from allergic conjunctivitis caused by airborne allergens (dust, animal hair, pollen) to allergic contact eczema.
Atopy can manifest as eczema (atopic skin malfunctions and over-reacts to its environment, becoming inflamed) as well as asthma, rhinitis, conjunctivitis, and more.
For more information, check out this in-depth overview of atopic eczema.
Skin care and treatments for eczema on the eyelids
A cortisone cream prescribed by your doctor will help soothe the intense itching associated with eczema. One common alternative for the eyelids, in cases where eczema tends to come back, is a tacrolimus ointment, which acts as a topical immunosuppressant.
For allergic (contact) eczema, identifying the allergen and removing it from your daily routine are also part of the treatment process.
For atopic eczema, you will also need to “repair” the skin. This can be achieved by applying an emollient: hydration is essential to treating atopic eczema.
What to do if your baby has eczema on the eyelids
You will need to determine whether baby has an allergy (contact eczema) or atopic skin (atopic eczema).
In the case of a contact allergy, a product applied to baby’s face may have caused the reaction. Babies are touched often, so you will need to consider a by-proxy contact eczema: perhaps baby is having an allergic reaction to a product handled by another person who then touched baby’s face.
Atopic eczema, when it affects babies’ faces, appears most often on the cheeks and forehead. In the case of atopy, several soothing habits can be adopted to relieve baby’s eczema and prevent flare-ups.
Is eczema on the eyelids caused by stress?
Stress does not cause eczema, period. At most, stress may be an aggravating factor or trigger for an atopic eczema flare-up, but the cause is atopic skin, which is genetic. Thus, eczema is not “all in your head”.

